UCLA Sport-Related Concussion Conference Part 1
On January 27, 2017, Melinda and I attended the first ever Sports-Related Concussion Conference at UCLA featuring the data from the NCAA-DOD study going on nationwide right now!
I believe this blog will have to be 2 or 3 parts due to the incredible content presented this weekend. Some of the data is ahead of print (peer-reviewed journals) so we will only be able to skim this data as we go along. It will be interesting to see how the information collected regarding the collegiate athletes and cadets will trickle down to the high school and youth sports athletes across the country.
That being said, let’s get started!
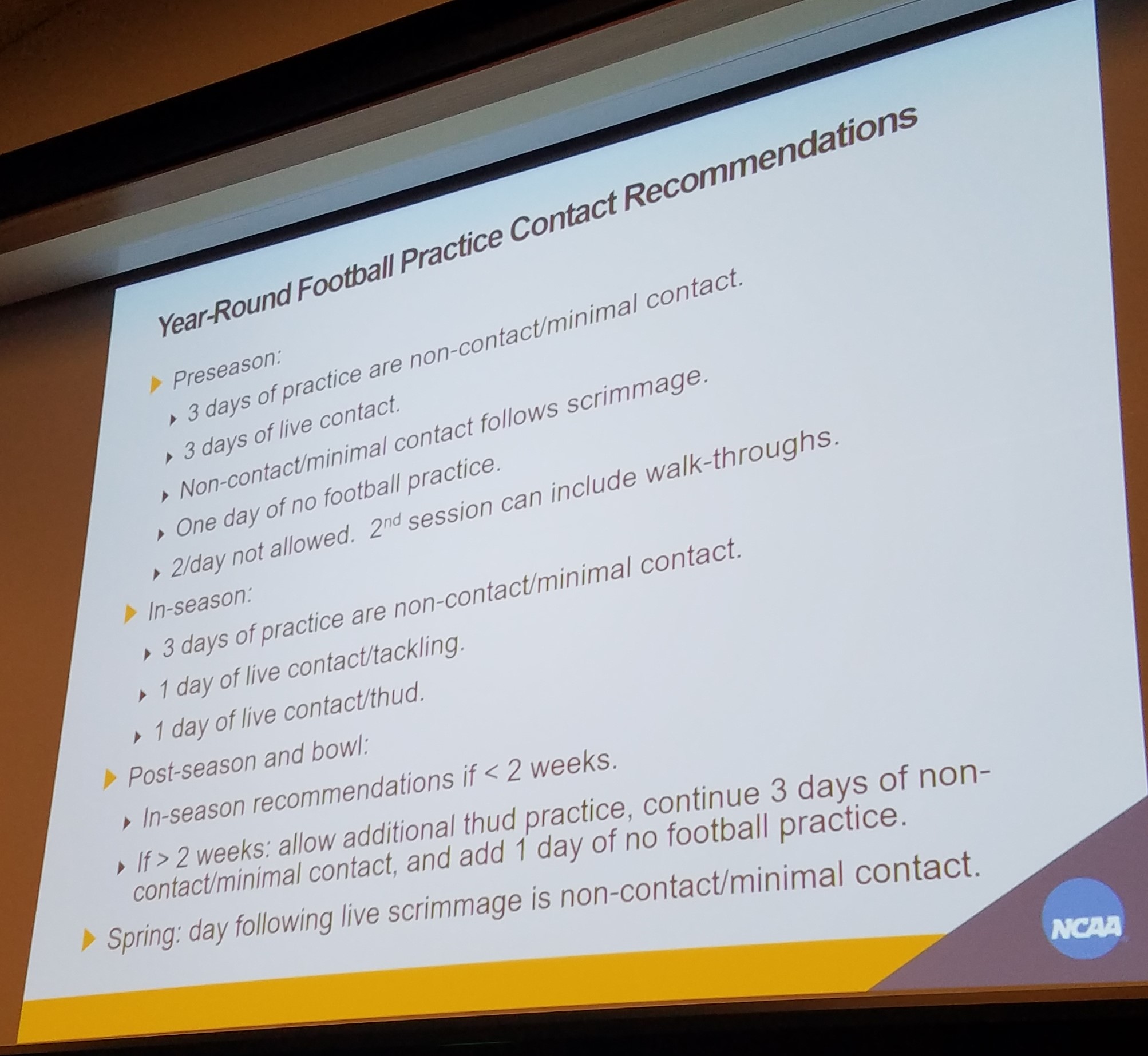
State mandated contact limits are a sure fire way to limit overall injuries, including concussions. Dr. Hainline presented his new research including the schedule in the photo above and most importantly, eliminating 2-a-days in football. These recommendations have been endorsed by 16 healthcare national organizations and 5 football organizations including USA Football and the NCAA Football Rules Committee.
According to Dr. Hainline, 58% of concussions in football occur during the pre-season in the month of August. If we limit the number of contacts, we will limit the potential for this high exposure to concussions. Studies have also shown no significant change in overall performance during the season with decreased frequency of contact practices.
We are so happy research is finally proving the thought that “if we limit contact, we will also limit injuries – including concussions.” Furthermore, research is disproving the proclamation “if the kids don’t practice enough, they’ll get hurt during the game from bad form.”
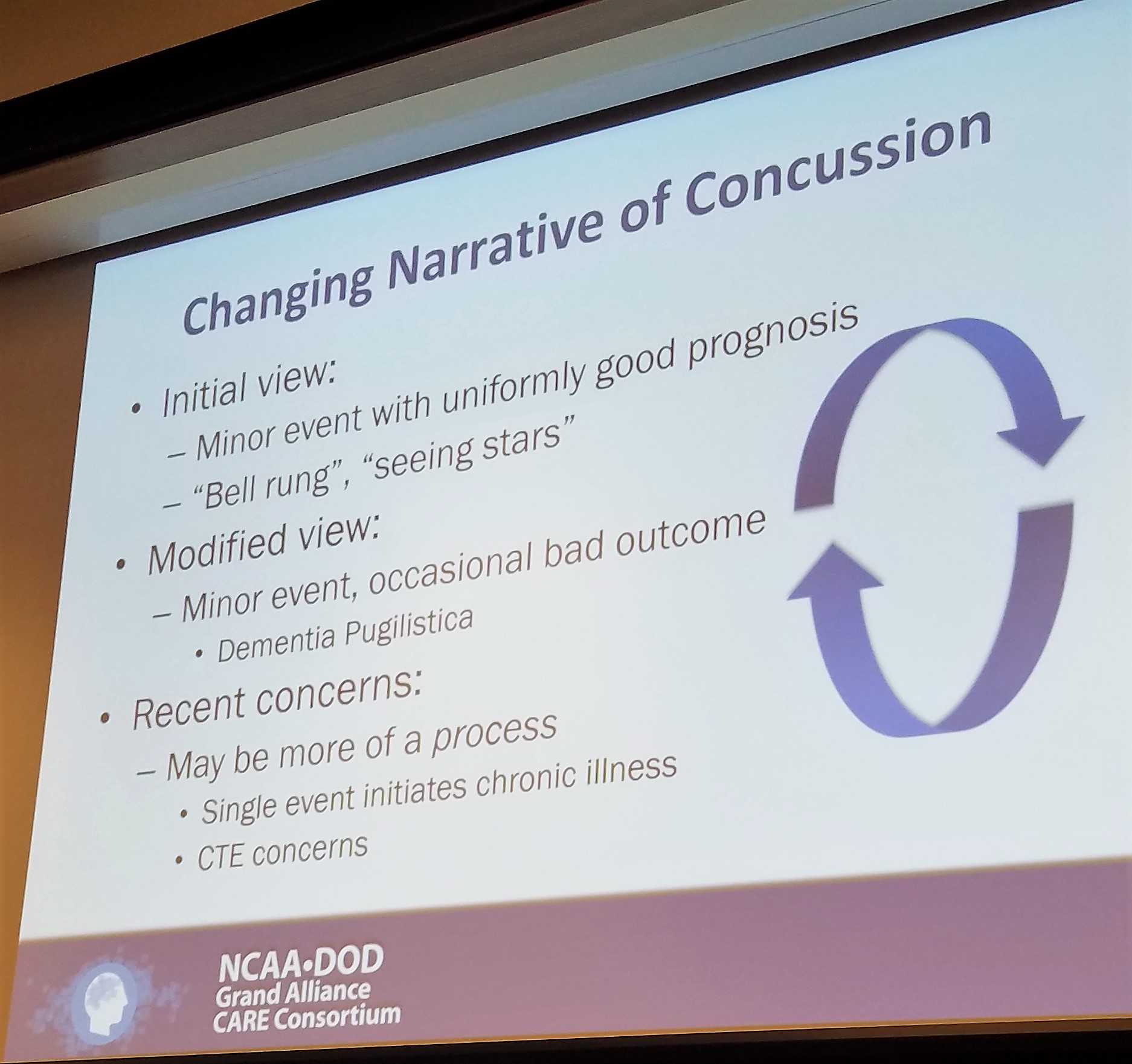
The science regarding concussions is ever evolving. We now know that there is no such thing as “getting your bell rung” and that the “stars” an athlete may see represent neurological changes in the brain due to contact.
In the following section we will talk about the new way the CARE Consortium would like us to look at concussions. A way that Phoenix fully supports and is proud to say we are already using!
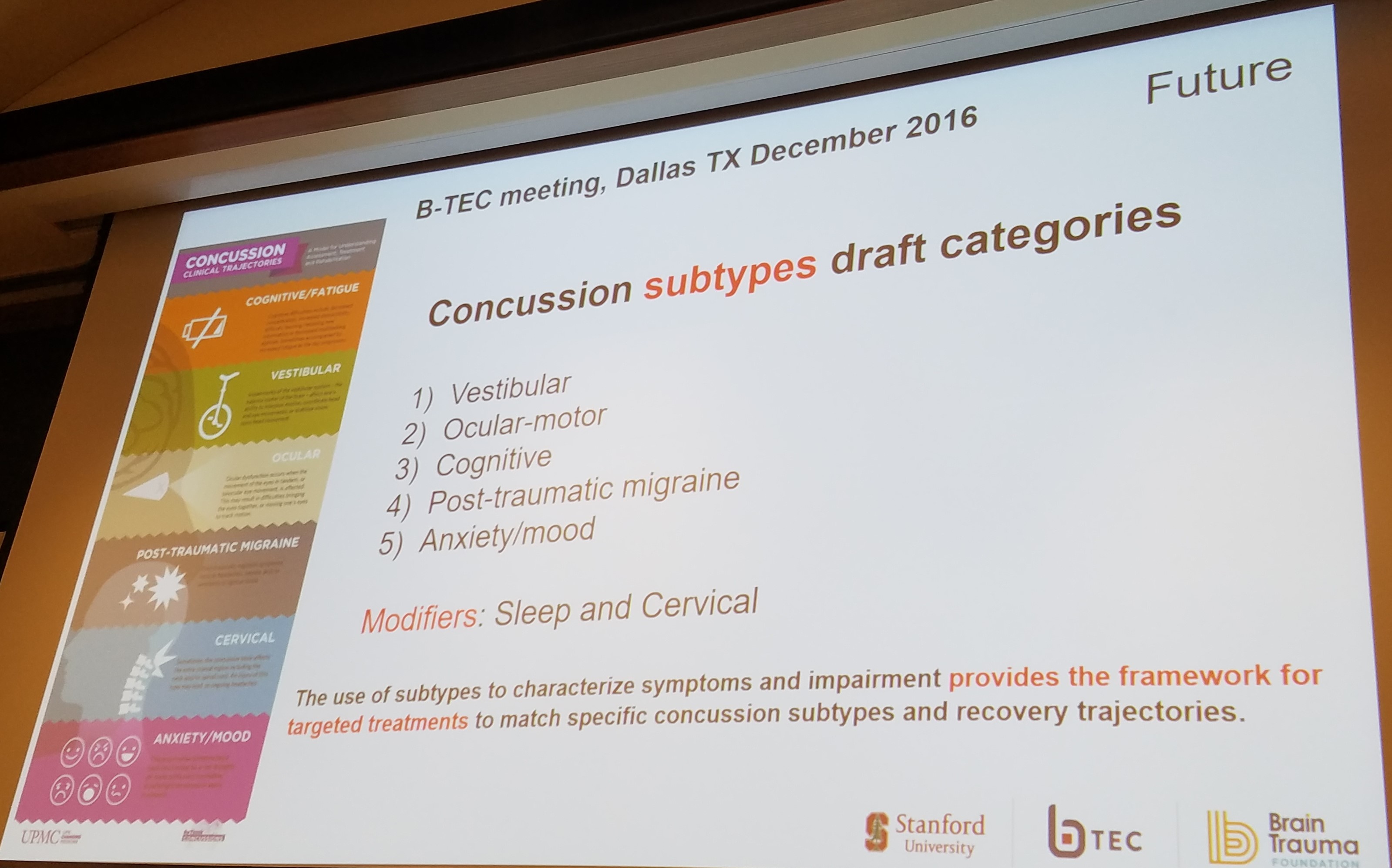
By treating concussions as a broad and generalized injury, we limit our ability to discover a targeted treatment protocols.
By classifying subsets of concussions – i.e., vestibular, oculomotor, or combinations of either, we allow ourselves to create treatment paradigms that will actually help patients in recovery!
For example, if you had an ankle sprain we would classify it by the ligaments injured. This allows us to treat you better. We need to create the same type of system for concussions.
We know there are clusters of symptoms and that a patient can even evolve into different categories throughout the course of a longer recovery. By isolating the subsets, patients will be able to receive the best treatment recommendations for their specific condition. We will be able to target treatments to the individual’s needs and thus people will recover better and quicker than ever before!
In our clinic, if a patient presents with vertigo AND oculomotor deficits, we always treat the vertigo first. What we have found is the patients get better faster and tolerate treatment better with the vertigo out of the way. By teasing out the subset and the primary/secondary subsets of a patient, we have been able to improve our recovery times.
At Phoenix, we are excited that the concussion world will be working hard to continue to research these subsets and create treatment guidelines for each subset!
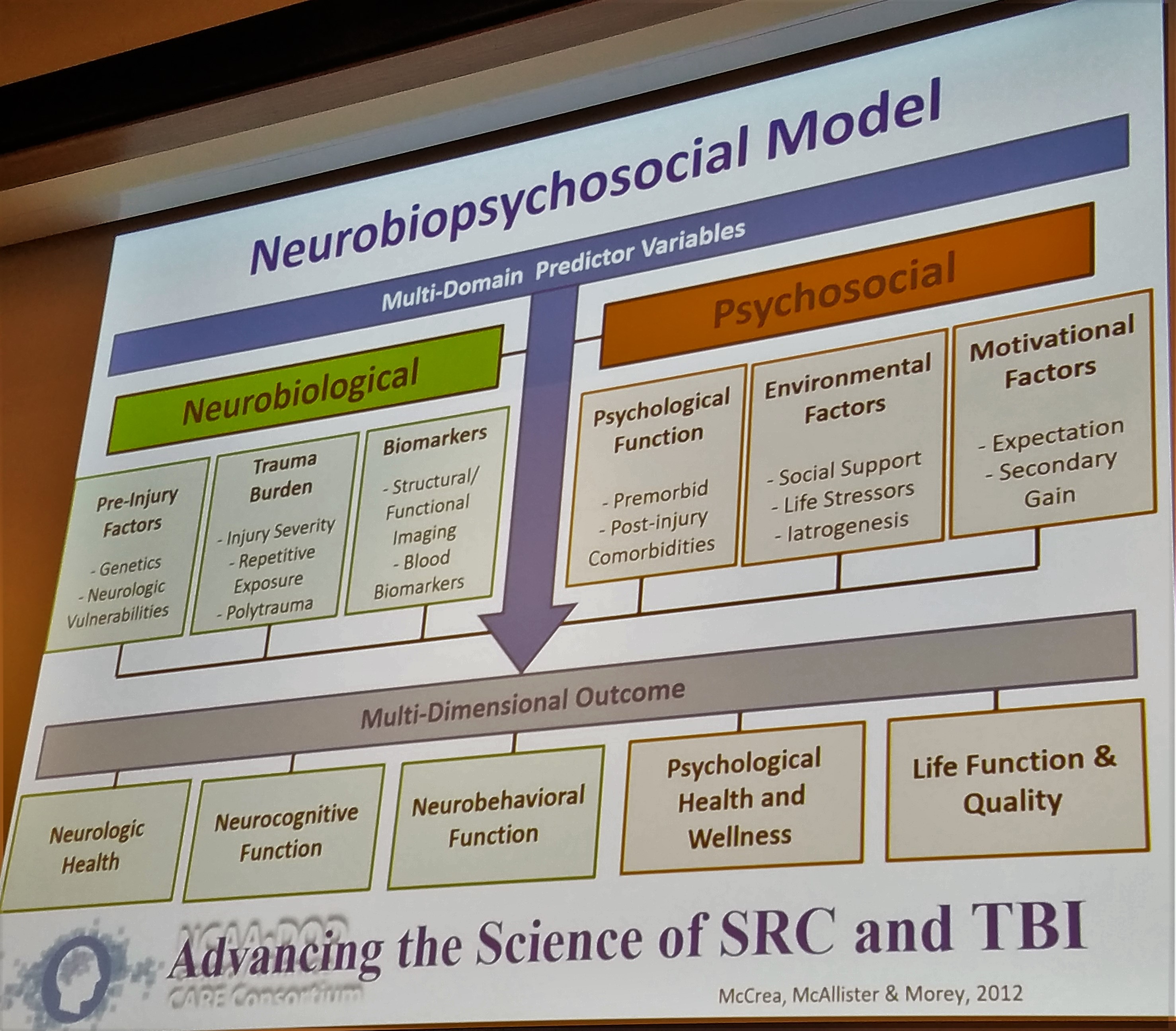
Why is each concussion so different? Glad you asked! Not only is each concussion different because of the different areas affected by different types of injuries, but also because each person is different!
Each person comes into their concussion with different neurobiological and psychosocial factors, as so elegantly described in the above slide by Dr. Thomas McAllister. Each person has their own history of concussions, genetics, support systems, mental health history, and motivational factors. The research is now starting to look further into how these factors play a role in both the severity of injury as well as the path of recovery.
It is important to consider the whole person when treating concussions and to know what sort of “baggage” that patient came in with. It is also important not to classify a person by their “baggage”. It is important healthcare providers do not see a patient with prior anxiety or depression and pigeon-hole that patient into a different trajectory solely for that reason. There will be responsibilities in this research to ensure that a patient profile can be created to help create a treatment plan. It is important to note that this profile should not limit a patient’s opportunities.
As for the most common symptoms post concussion, the research continues to suggest that headaches, dizziness, visual deficits (oculomotor), and sleep / behavior / and cognitive deficits are at the top of the list.
We all come into our concussions with our neurobiological and psychosocial factors causing our injuries to affect us in different ways. The research now needs to focus on how to define subtypes of concussions based on these common symptom collections. Once we can determine the subtype, treatment guidelines will not be far behind.
It may seem like there is still so much to learn, but you shouldn’t feel discouraged. The realm of concussion research has come so far in the last 10 years and we are on the cusp of huge breakthroughs in the next 5 years. As Phoenix and similar organizations continue to progress their treatments and the researchers continue to collect data; we will all be able to put the puzzle pieces together!
It is an exciting time for concussions and there will eventually be a clear solution to the concussion treatment problem. But to get there, we have to fully understand what in the world we are dealing with!
Check back in about 1 week for part 2 of the conference where we will discuss the biomechanics of concussions and what exactly is happening in your brain during a concussion. I will try to make it as exciting as possible!
Don’t forget to sign up for our newsletter at the bottom of the page!


Hi! I’ve been following your web site for a long time now and finally got the bravery to go ahead
and give you a shout out from New Caney Texas! Just wanted to tell you keep up the good job!
Thanks Jim! I appreciate the feedback. Check back for our next post!